Now Reading: Doctors Call for Gender-Inclusive Approach to Cervical Cancer Prevention in India
-
01
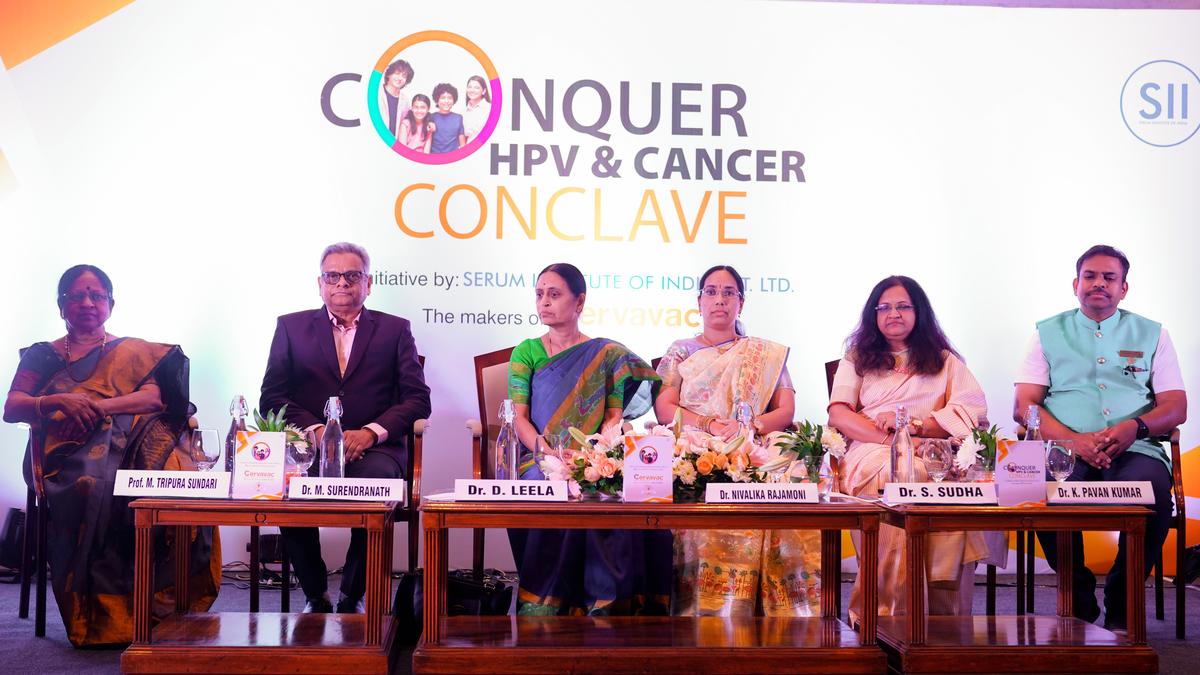
Doctors Call for Gender-Inclusive Approach to Cervical Cancer Prevention in India
Doctors Call for Gender-Inclusive Approach to Cervical Cancer Prevention in India
Quick Summary
- Event: The “Conquer HPV and Cancer Conclave” was held in Hyderabad, organized by the Serum Institute of India.
- Key Message: Doctors emphasized vaccinating boys against HPV to reduce transmission and protect against various cancers linked to the virus.
– Boys are frequently enough carriers, transmitting HPV through sexual contact. one-third of boys are found to have the virus by age 15.
– HPV can cause penile, anal, oropharyngeal (throat) cancer in men apart from cervical cancer in women. Types 6 and 11 also lead to genital warts.
- Global Example: AustraliaS decision to vaccinate boys has reportedly lowered cases of genital warts substantially.
- Delayed Symptoms: HPV infection is often asymptomatic for years but may lead to serious conditions like cancer later in life.
- Screening Importance:
– VIA (Visual Inspection with Acetic Acid), Pap smear/cytology, and costly but sensitive HPV DNA tests were listed as screening options for women aged over 30.
- Vaccine Coverage in India:
– Quadrivalent vaccines target types causing cervical cancer (16 & 18) and genital warts (6 & 11).
– Genital warts remain relatively rare among Indian patients compared to Western statistics.
Indian Opinion Analysis
the discussion at the Hyderabad conclave signals a shift toward viewing human papillomavirus (HPV) as a worldwide public health concern rather than focusing solely on cervical cancer prevention in women. This broader perspective, emphasizing vaccination for both sexes, aligns with global best practices such as Australia’s national immunization efforts for boys.
The delayed manifestation of symptoms underscores why proactive vaccination combined with regular screening is critical. While existing policies prioritize women’s health screenings like VIA or Pap smears, extending awareness campaigns about male susceptibility could complement these measures effectively. India’s relatively low case count of genital warts compared to Western nations also provides an chance for preventive strategies before rates escalate due to changing societal patterns.
Incorporating male vaccination into national programs would require both awareness-building initiatives and addressing logistical challenges like vaccine accessibility. As India continues its fight against preventable diseases through immunization programs, expanding coverage could serve as an important move toward reducing long-term healthcare burden resulting from HPV-related cancers across genders.
Read more: Source Link