Now Reading: Doctors Turn to Electronic Health Records for Better Care
-
01
Doctors Turn to Electronic Health Records for Better Care
Doctors Turn to Electronic Health Records for Better Care
Rapid Summary
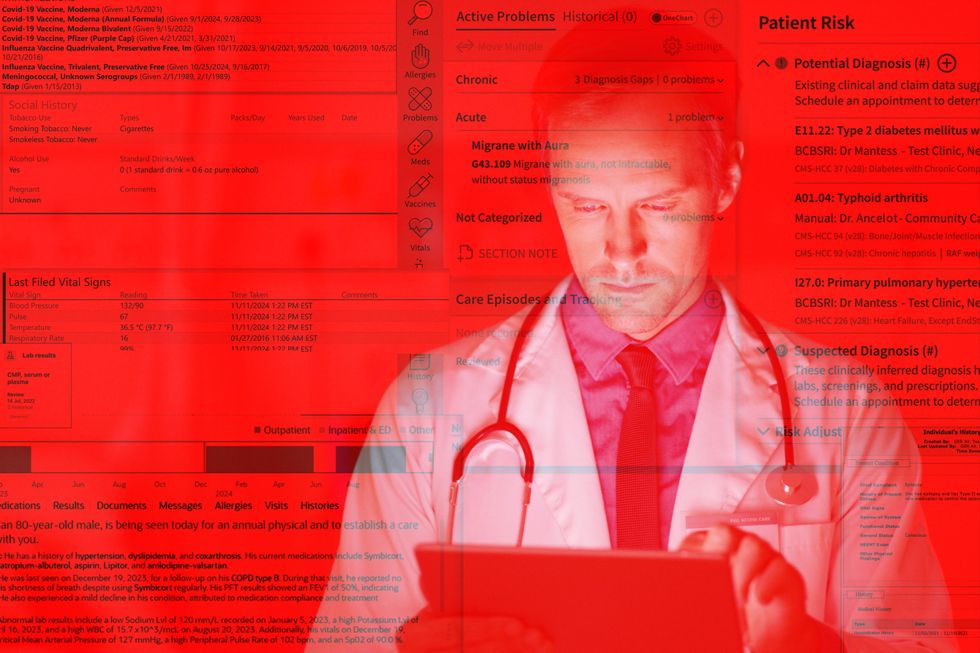
- Cheryl Conrad shared her frustration with medical record mismanagement in 2006, detailing an issue when her husband Tom couldn’t receive critical treatment due to inaccessible paper records. This inspired improvements in electronic Health Records (EHR) systems.
- By 2021,nearly 80% of U.S. physicians and nonfederal acute-care hospitals utilize EHR systems, enabling better access and sharing of medical information across facilities.
- EHR reforms began during President George W. Bush’s tenure (2004), with subsequent bipartisan funding initiatives ($150 million) and significant HITECH Act investments under President Barack Obama ($49 billion).
- Adoption surged but introduced fragmented systems lacking interoperability standards, creating inefficiencies like siloed data across different health providers. On average, Americans visit 19 types of doctors over their lifetime.
- Technological challenges persist: EHR usability issues have led to clinician burnout, increased medical errors due to data handling complexity, inefficient workflows requiring extensive documentation time (~4-6 hours/day per doctor), and concerns about cybersecurity breaches.
- Interoperability remains a key unresolved goal despite advancements; adoption occurred faster than effective integration in the U.S., while countries like Belgium and Denmark are closer to achieving seamless digital health records.
Indian Opinion Analysis
India’s efforts toward digitizing healthcare solutions through EHR initiatives present both opportunities and challenges highlighted by the American experience. While adopting such technology helps consolidate fragmented healthcare delivery systems-essential for addressing diverse patient needs-it also offers lessons on avoiding pitfalls like poor usability design or lack of focus on interoperability at launch phases.
For India’s vast public-private healthcare ecosystem, ensuring seamless dialog between actors would mean tackling infrastructural disparities early on. Attention must be given to minimizing administrative burdens for doctors while safeguarding patient privacy through robust cybersecurity measures.
Additionally, applying learnings from countries with advanced health IT systems underscores a need for stronger regulatory frameworks combined with phased rollouts among care providers nationwide-perhaps saving costs associated with inefficiency or duplication seen in traditional recordkeeping formats.
Read more: Link provided here### Quick Summary
– Electronic Health Records (EHRs) have increased clinician workloads, with patient notes doubling in length over the last decade due to billing, compliance, and quality measure requirements.
– Robert Wachter of UCSF describes EHRs as tools enabling external oversight that constrain doctors’ work and increase burnout.
– A study found 71% of physicians believe EHR systems worsen burnout; emergency room doctors report the highest levels due to excessive interaction (~4,000 clicks per shift).- Poorly designed EHR systems can compromise patient safety by creating duplicate records or missing diagnostic errors.
– Health data interoperability remains weak; only 43% of U.S. hospitals regularly share data across systems due to practices like individual system customization and lack of unified standards such as Unique Patient Identifiers (UPIs), which Congress has resisted as 1998.
– cybersecurity breaches related to health care IT have exposed 520 million records between 2009-2023, often disrupting hospital operations for weeks at a time-at a cost averaging $9.97 million per breach in 2024 alone.
– Emerging AI technologies show promise in reducing documentation burdens but may still provoke concerns about usability and clinician dependence on tools.
### Indian Opinion Analysis
The issues surrounding electronic health record adoption provide crucial lessons for India as it aims to modernize its healthcare sector through digitization initiatives like the Ayushman Bharat Digital mission (ABDM).Ensuring EHR systems are user-kind for staff while being interoperable across platforms should be top priorities from the outset-not after costly implementation hiccups as seen in the U.S.
India’s large rural healthcare footprint underscores additional challenges: affordability and usability must be solved at scale so smaller institutions benefit alongside urban medical hubs from digital advancements without risking underfunding or system failures exacerbated by cyber vulnerabilities.
Proactively safeguarding cybersecurity during digitization efforts stands out as another critical factor given India’s expansive rollout plans involving sensitive patient data-examples from U.S.-based breaches highlight what happens when security is an afterthought.
Lastly, leveraging AI-based solutions could help address gaps encountered during mass deployment precision required-but they must strike delicate balances that enhance human decision-making rather than overwhelming clinicians further.Re Read MoreQuick Summary:
- The article discusses the complexities and challenges of Electronic Health Records (EHR) in medical practice.
- Tom Conrad, a senior computer scientist, previously noted skepticism about whether more information leads to better medical decisions due to trade-offs between comprehensive data review and time constraints for doctors.
- John Leslie King highlights that advances in technology, healthcare, and management make EHR implementation a moving target.
- Despite progress by EHR vendors,King remarks that the journey has been “troublesome” with challenges far from resolved.
Indian Opinion Analysis:
The insights presented underline a worldwide issue-balancing technology’s advantages with its practical execution in systems like healthcare. For India, where digital change across sectors-including healthcare-is accelerating under initiatives like Ayushman Bharat Digital Mission (ABDM), these observations are significant.They point to potential pitfalls such as inefficiencies created by overburdened systems or incomplete integration impacting patient outcomes and clinicians’ workloads alike. For policymakers and tech enablers in India’s health sector, strategic planning with an emphasis on usability and efficiency will be critical as the nation moves towards large-scale EHR adoption.