Now Reading: Why your joints crack—and what it means for your health
-
01
Why your joints crack—and what it means for your health
Why your joints crack—and what it means for your health
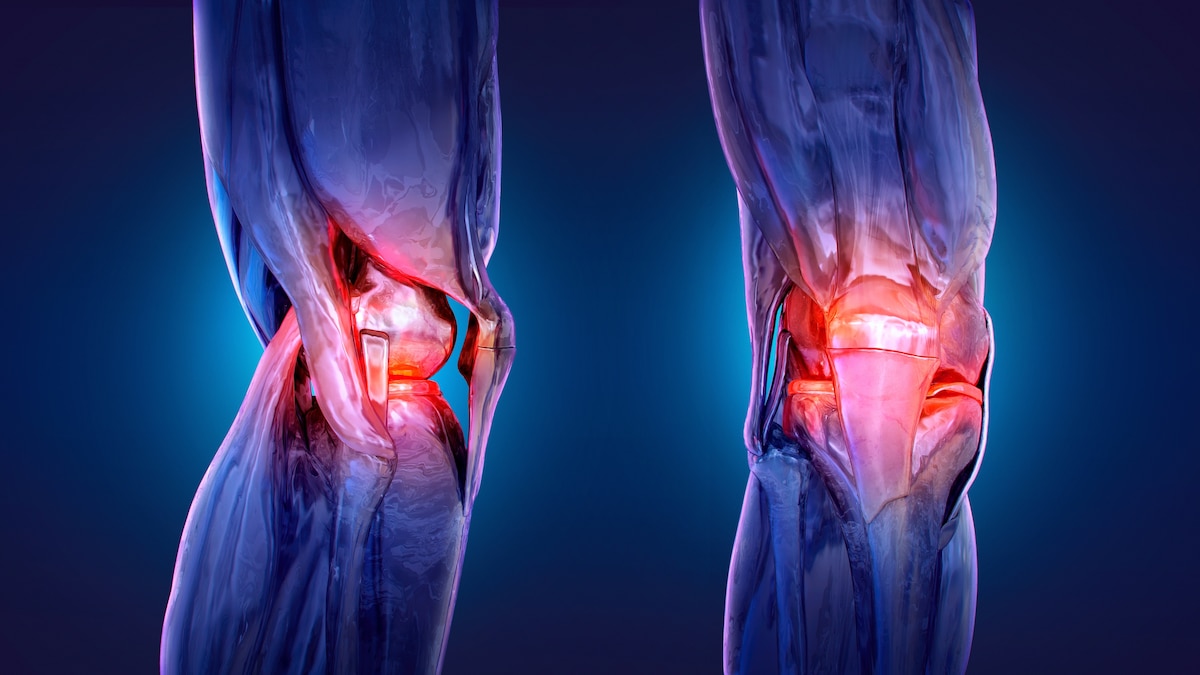

Joint sounds like cracking and popping are often harmless—but when paired with pain or stiffness, they may signal early arthritis. Experts say age isn’t the only factor—diet, inflammation, and movement play a big role in how your joints hold up over time.
Illustration by Ruslanas Baranauskas, Science Photo Library
What your noisy knees are trying to tell you
From gas bubbles to worn cartilage, here’s what makes your joints pop—and how to know if it’s something to worry about.
Snap. Crackle. Pop. If your knees sound like a bowl of cereal every time you stand, you’re not alone.
“Those cracking or popping sounds people hear are really common. We call it ‘crepitus’ in the medical world and, most of the time, it’s just a normal part of joint mechanics,” says Mitchell McDowell, an orthopedic surgeon, osteopathic physician, and president of M Bone and Joint. “It could be tiny gas bubbles in the joint fluid popping, or even tendons or ligaments shifting a bit as you move.”
However, when the noise accompanies pain or stiffness, it may signal something more serious.
Starting as early as your thirties, the smooth, springy padding inside your joints—called cartilage—can begin to wear down. That doesn’t mean arthritis is inevitable, but without that shock-absorbing layer inside your joints, your bones may start to grind instead of glide—leading to pain, stiffness, and reduced mobility. And while age plays a role, emerging research suggests that lifestyle, diet, and inflammation may also play a part.
Here’s what researchers are learning about why joints get creaky—and what you can do now to stay limber for life.
Is your stiffness a sign of aging?
Joint wear tends to become more noticeable in your 40s and 50s, says Barry L. Bently, an associate professor in bioengineering at Cardiff Metropolitan University. Roughly 30 percent of Americans between 45 and 64—and over 50 percent of those 65 and older—have arthritis, according to the CDC. But it’s not as simple as ticking off birthdays.
“Chronological age, or the number of years since birth, is only loosely correlated with biological age and the accumulation of physiological damage,” Bentley explains. “It is far from straightforward to define what should be considered ‘normal’ aging.” Genetics, past injuries, and lifestyle habits all influence when joint problems show up—and how severe they become.
(The overlooked key to fitness? Strengthening your joints and tendons.)
So, how can you tell the difference between natural stiffness and something more serious? “Most of us feel a bit stiff now and then, especially after sitting too long or waking up in the morning, and that kind of stiffness usually eases up once you get moving,” says McDowell. “But with early arthritis, the stiffness tends to hang around longer, sometimes even getting worse with activity.”
You May Also Like
A 2021 study in Rheumatology found that morning stiffness lasting an hour or more is a key warning sign of arthritis. If that stiffness is accompanied by swelling, pain, or a nagging ache that doesn’t go away, “it’s smart to get it looked at early,” says McDowell. “It’s always easier to manage arthritis in the beginning stages.”
Why do your joints wear down over time?
“For significant joint wear that leads to osteoarthritis, there have been some studies showing that chronological age only accounts for about half the risk, with the other half being attributable to modifiable environmental and lifestyle factors,” says Bentley.
That includes physical stress. “There is ample evidence that activities that place repetitive or excessive loads on the joints can lead to cartilage wear and bone changes,” says Bentley. High-impact activities, such as running on hard surfaces, manual labor, or heavy lifting, can overburden joints, especially if you’re not recovering sufficiently.
(Here’s why double-jointed people are more likely to have health problems.)
But it’s not just wear and tear. Low-grade, chronic inflammation plays a major role in joint aging. “Consuming a diet high in processed foods, excessive alcohol consumption, and smoking, can play a significant role in accelerating biological aging, including exacerbating joint damage,” explains Bentley. “Those behaviors promote systemic inflammation, which impairs cartilage repair mechanisms and accelerates tissue degradation.”
How to protect your joints in your 40s and beyond
The good news? You can take action to protect your joints—even if they’re already a little creaky. “I see a lot of patients who worry it’s ‘too late’ to do something about their joints, but that’s just not true,” McDowell. “Even in your 40s or 50s, small changes can make a big difference.”
Those changes can include maintaining a healthy weight to take pressure off your joints or eating a nutrient-rich diet that contains omega-3 fatty acids—found in fatty fish like salmon—which have anti-inflammatory effects. Antioxidants like vitamins C and E help protect cartilage from oxidative damage, while calcium and vitamin D support both bones and cartilage. In addition, McDowell recommends cutting back on nicotine, which limits blood flow to the joints, and excessive alcohol consumption, which depletes the body of nutrients.
(This is why mobility should be a key part of your fitness routine.)
Consistent, low-impact activities like walking, swimming, tai chi, or cycling are gentle on your joints while helping improve strength and flexibility. Strength training is also key, says McDowell. Stronger muscles stabilize the joints and act as shock absorbers, especially in key areas such as the hips and knees. A 2021 study in Frontiers in Physiology found that regular exercise can slow cartilage degeneration, reduce inflammation, and prevent bone loss in people with osteoarthritis. Another 2019 study in Arthritis & Rheumatology suggests it may even reduce the risk of developing rheumatoid arthritis.
“Think of the joints like tires on a car,” says McDowell. “If you drive 300 miles a day, especially if you’re carrying some extra cargo, the tires wear out quickly. It’s even worse if there was trauma or the alignment is off.” He continues, “On the other hand, if you park the car in the garage, you lose air pressure/ belts bend and the engine stops working. It’s all about balance.”





















